
The Challenge: Rural populations in Kenya lack adequate access to affordable, high quality healthcare. While the challenges of providing healthcare in this setting are many, patients consider proximity and cost the greatest barriers to accessing the care they need.
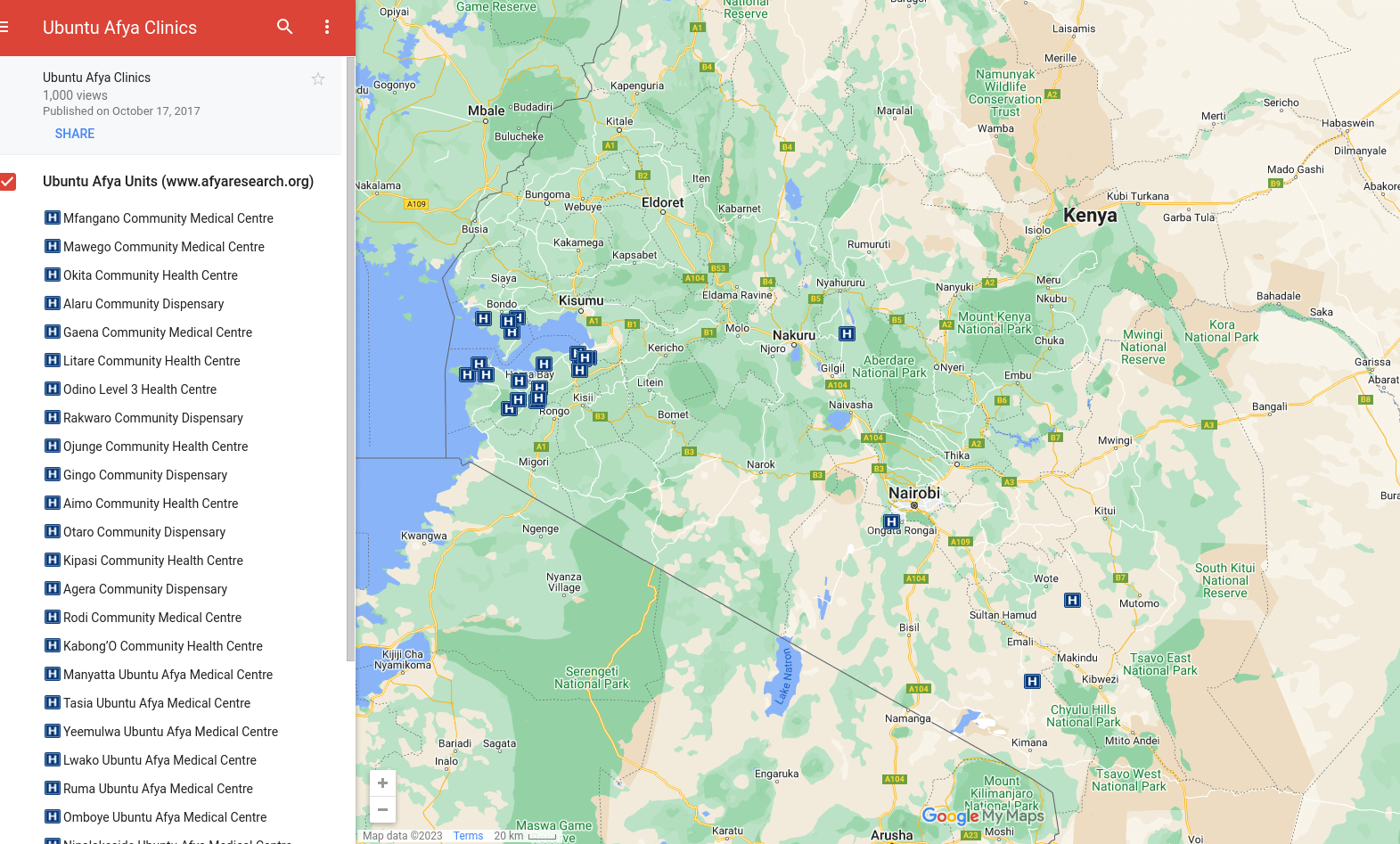
Our Strategy: Set-up and manage Ubuntu Afya Medical Centres in rural areas where there is a dearth of public and private healthcare options.
The Innovation: Core to our model is the engagement of partner communities to set-up, co-own, and co-operate our medical centres. We believe that by engaging communities in the health system we improve the relevance of our services, patient trust and loyalty, and encourage community ownership over available healthcare services.
Sustainability: Sixty percent of Ubuntu Afya Medical Centres break even within the first 12 months of launching, a measure of sustainability that has eluded other private sector players working with our target population. Centre sustainability is supported by subsidizing the cost of care with revenue from transport and financial service enterprises set-up and operated by partner communities. Not only does this make care more affordable, it supports financial inclusion and addresses other healthcare access challenges in the community.
Impact:
- Each medical center services a catchment population of approximately 5,000 people
- Two-thirds of our patients are women and children
- 12 medical centers support child delivery services
- Offering treatment for non-communicable diseases, preventing catastrophic healthcare spending often tied to this type of care
Cost: Set-up and operating costs for 1 medical center for 1 year equal approximately $1 per capital.

The Challenge: In Kenya we lack locally appropriate and affordable health information and clinic management systems that can be utilized across disease verticals and at all levels of care. This has excluded the majority of patients and providers in Kenya from accessing the benefits of health technologies and prevented comprehensive collection of national health data to aid in decision-making.
Our Strategy: Develop and deploy a health information and medical records system that can be adopted by those without access to the benefits of health technologies as well as more advanced healthcare providers. We believe that by bringing the benefits of health technologies to providers delivering the majority of healthcare in Kenya, we can improve quality of care for patients and existing health databases and reporting systems for improved decision-making.
The Innovation: Stone HMIS® operates across diseases verticals and at all levels of care. It is amenable to various platforms and is an open-source system that facilitates uptake and flexibility as the health system grows and changes. Stone HMIS® has been designed to align with the work-flow of providers in Kenya and is interoperable with existing health databases and reporting systems.
Sustainability: Stone HMIS® is a freeware technology, supporting its potential for growth and impact in the coming years. Sustained impact will come from health data generated by the system and decreases to costs of development over time.
Impact:
- Improve clinic management for effective and sustainable care
- Support best practice healthcare and decision-making for higher-quality care
- Contribute to national health data collection and reporting systems to inform public health interventions
Cost: Implementation of the system is anticipated to improve efficiencies and reduce costs for the healthcare provider and the broader health system. Our impact evaluation is tasked with putting exact numbers to these efficiencies and cost savings.

The Challenge: Too often health research is removed from the practice of providing care and health workers who can use their knowledge to inform research projects and benefit from deploying research findings.
Our Strategy: We partner with research institutions and health and development agencies to bring evidence to the forefront of healthcare provision.
The Opportunity: We are uniquely able to leverage our network of medical centers for health research. As our network and patient population grows we see opportunities for engaging third parties in health research conducted through our network of medical centers.
Sustainability: We are compensated for our monitoring and evaluation and evidence synthesis and training work. Our Research and Evidence Program is a net contributor to the organization’s bottom line and is able to subsidize growth and development in our other major programs: the Ubuntu Afya network and Stone HMIS.
Impact:
- Supporting monitoring and evaluation for Gertrude’s CICF funded M-Wallet Conditional Cash Transfer Program in Northeastern Kenya
- Supporting monitoring and evaluation of our own Ubuntu Afya work in Homa Bay, Kenya
- Led monitoring and evaluation of the Tele-Afya telemedicine pilot program for CISCO Systems and other partners
- Analyzed Kenya’s DHIS2 reproductive health data in partnership with the University of North Carolina’s MEASURE Program
- Ongoing completion of systematic reviews on specific health topics in partnership with Kleijnen Systematic Review Systems
- Ongoing training in evidence review and incorporation into health practice in partnership with JBI, University of Adelaide, Australia.
Homa Bay County, Kenya
In 2016 Afya Research Africa partnered with DFID’s County Innovation Challenge Fund and the Homa Bay County government to expand the Ubuntu-Afya network in Homa Bay County. In one year, the Afya Research Africa team set up 16 new medical centers working closely with the County Health Management Team to identify viable sites that would complement government-run facilities. Afya Research Africa also helped the Homa Bay County Health Management Team map and installed STONE HMIS in county health facilities, an effort to improve healthcare decision-making with the use of data.
Turkana County, Kenya
In 2017 Afya Research Africa partnered with the Turkana County Government to create a virtual network of healthcare providers using STONE–HMIS® in Turkana County. STONE–HMIS® is a modular system that serves all the components of the health system continuum, including community, administrative, clinical, pharmacy, and laboratory modules. We have developed new capabilities in STONE–HMIS® for communication, education, and biometric-based unique identification of mothers, and provider collaboration for better care and outcomes. We implemented a digital connection of MNH providers and their target CHUs using STONE–HMIS®: the Ubuntu Digital Collaboration (UDC). Utilizing Stone HMIS®, community health workers and Maternal and Newborn Health (MNH) providers are able to uniquely identify, educate, empower, and offer individualized intervention and follow-up pregnant women who are highly mobile and tend to seek care across different facilities in settings with difficult access to health services. This has increased the utilization and quality of MHH services. Utilizing machine learning to analyze provider-client interactions, we have empowered healthcare providers to discern risk factors for complications associated with early motherhood and attendant pregnancy outcomes and facilitate anticipatory interventions.
Garissa County, Kenya
Afya Research Africa’s Research and Evidence team partnered with Gertrude’s Children’s Hospital to evaluate the effectiveness of the M-Wallet project in Garissa County. The Garissa M-Wallet project is a conditional cash transfer program that supports access to MNH services and incorporates a telemedicine program to support referrals across different clinical domains. The project has been associated with significant improvement in MNH access indicators in intervention settings that previously had challenges with access.
